Why Algeria, Azerbaijan, Belarus, Brazil, Bulgaria, China, Colombia, Kazakhstan, Mexico, Romania, Russia, and Turkey must issue compulsory licences on dolutegravir now.
At the 10th IAS Conference on HIV Science, the World Health Organization (WHO) recommended, today (21 June 2019), that all countries immediately adopt dolutegravir-based regimens as the preferred first-line treatment for HIV.
However, unless urgent action is taken, the WHO’s recommendation is likely to be undermined by patent barriers in upper middle income countries (UMICs). Forty-nine UMICS excluded from voluntary licenses (VLs) issued by ViiV Healthcare must act now in order to access DTG: at least twelve of these countries must issue a compulsory license (CL).
The International Treatment Preparedness Coalition (ITPC) and the Global Network of People Living with HIV (GNP+) urges the 12 countries[1] to exercise their right to use a compulsory license, which is a legal procedure authorized by international agreements and national laws. A CL will allow these countries to access more affordable generic versions of DTG existing today, and to comply with WHO recommendations.
Benefits of dolutegravir (DTG)
The WHO has confirmed that DTG results in faster viral suppression, fewer side effects and a high genetic barrier to resistance. DTG improves the quality of life among people living with HIV.
Countries benefit from DTG too: DTG can overcome the increasing prevalence of HIV drug resistance and simplify procurement processes. DTG-containing regimens have been the standard of care for HIV treatment in high income countries and utilized successfully in the US and Europe for more than 300,000 patients since 2015.
The importance of ensuring universal access to affordable DTG-based regimens has also been underscored by the recently released 2019 Global Epidemic Update by UNAIDS[2] which highlights the increase in HIV infections in precisely the regions from which UMICs have been excluded from the VL. According to UNAIDS, “the annual number of HIV infections has increased in three regions: Eastern Europe and Central Asia (29% increase), Middle East and North Africa (10% increase) and Latin America (7% increase)”.[3]
Exclusions for adults and children up until 2031
Access to DTG-based regimens in low and middle income countries is being dictated by patent barriers. ViiV has filed for, and been granted, multiple evergreening patentson DTG, claiming and extending their exclusive rights on DTG and DTG-based regimens in several countries until at least 2026, in some cases until 2031.
In 2014, ViiV Healthcare signed a bilateral voluntary licence (VL) with a generic company covering 92 countries.[4] That same year ViiV also signed separate VLs with the Medicines Patent Pool (MPP) allowing generic producers to manufacture adult and pediatric generic versions of DTG: the adult ViiV-MPP VL covered all low income, all least developed and all sub-saharan African countries. Exclusions from the pediatric license were more limited but still left out key upper middle income countries. In 2016, the adult licence territory in the MPP VL was extended to 92 countries. In 2018, two more countries were added to the MPP VL territory.[5] At present, 49 UMICs are excluded from the adult license and 9[6] from the pediatric license.
“Hide and seek approach to licensing”
“ViiV has been playing hide and seek with dolutegravir through their piecemeal approach to licenses. With WHO’s recommendation today, countries excluded from the VLs have to end this waiting game and take action now. As civil society organizations, we have confirmed that all low and middle income countries will be able to access a USD75 price for a DTG-based regimen if they remove the patent barriers,”says Othoman Mellouk, ITPC’s Intellectual Property and Access to Medicines Lead.
Mellouk is referring to the pricing agreement[7] brokered by the Clinton Health Access Initiative (CHAI) and others in 2017 for generic companies to offer a price of USD75 per person per year for public sector purchasers for a combination of dolutegravir, lamivudine and tenofovir (TLD). However, the offer appeared limited to only those countries included in the MPP voluntary license despite the fact that the VL includes provisions that allow supply to countries outside the territory if no patents are infringed or to countries where compulsory licenses have been issued. In January 2019, CHAI finally confirmed to ITPC that the price would be available to all low and middle income countries filling these two conditions.
140x price hike
“This confirmation is critical for upper middle income countries who have been struggling with protracted negotiations with ViiV on the pricing of DTG,” said Andrew Hill from the University of Liverpool.
In 2018, Andrew Hill and Joel Sim published results of an analysis of DTG pricing across 52 countries. They found that the median price of DTG[8] in countries excluded from VL agreements was more than 140 times higher ($8718) compared to countries which are included ($60). They also found that DTG prices compared to efavirenz in several upper middle income countries, varied from 0% higher (in Brazil) to 6889% (in Colombia).[9]
“ViiV has excluded several countries in Latin America from its VLs and as a result we are seeing exorbitant prices across the region. For Mexico, the host of this year’s IAS conference, dolutegravir is priced at USD2629 per person per year compared to USD143 for efavirenz; a price difference of 1738%. Already, over 80% of the Mexican government’s spending on ARVs goes to patented medicine,” said Alma de Leon, Treatment Activist and Regional Director of ITPC LATCA. “Procuring affordable generic versions will be critical to sustain Mexico’s commendable progress in achieving 90-90-90 and we call on Mexico to take the lead in our region and immediately issue compulsory licenses on DTG and DTG-based regimens.”
Routes to access
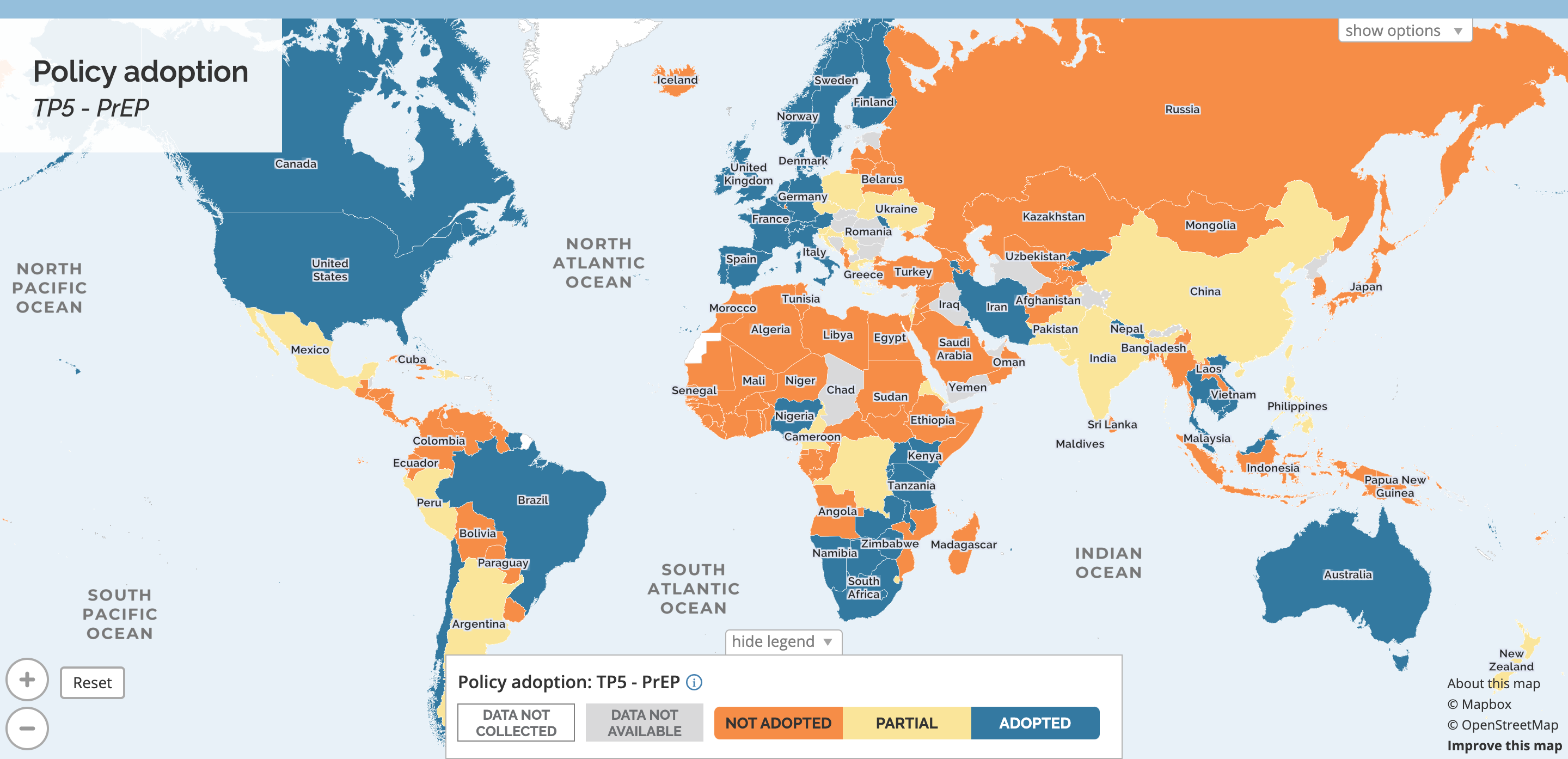
Twelve upper middle income countries[10] have patent barriers that may block generic versions of DTG and/or tenofovir/lamivudine/dolutegravir (TLD).
For these countries, there are several options for immediate generic supply. Under the Viiv-MPP VL, generic companies who have taken the license are authorized to supply to these excluded countries if they issue a compulsory license. So far there are 17 generic companies and product developers who have taken the license[11], 3 have WHO pre-qualification (PQ) for the DTG 50mg tablet and 2 have WHO PQ for the TLD combination.[12] At the same time, several of these upper middle income countries also have significant local production capacities that can be harnessed for the purposes of the CLs.
ITPC and GNP+ therefore call on the governments of: Algeria, Azerbaijan, Belarus, Brazil, Bulgaria, China, Colombia, Kazakhstan, Mexico, Romania, Russia, and Turkey; to issue compulsory licences on all patents covering DTG. ITPC and GNP+ also call on other UMICs excluded from the VL that have no patent barriers to immediately start procurement for generic DTG and DTG-based combinations.
“We are witnessing a situation similar to 20 years ago where people were either receiving treatment or not depending where they come from. This is unacceptable and countries must act now and issue compulsory licenses,” said Rico Gustav, Executive Director of GNP+. “The use of integrase inhibitors like DTG is now the standard of treatment for people living wit HIV. With the WHO recommendation; ready generic supply options; and a universally affordable generic price, the stars have been aligned for compulsory licensing by these countries.
Notes:
What did the WHO recommend?
First-line ARV drug regimens for HIV treatment:
Dolutegravir (DTG) in combination with an NRTI backbone may be recommended as the preferred first-line regimen for people living with HIV initiating ART.
- Adults and adolescents (strong recommendation, moderate-certainty evidence).
- Infants and children with approved DTG dosing (conditional recommendation, low-certainty evidence).
Second-line ARV drug regimens for HIV treatment:
DTG in combination with an optimized nucleoside reverse-transcriptase inhibitor backbone may be recommended as a preferred second-line regimen for people living with HIV for whom non-DTG- based regimens are failing.
- Adults and adolescents (conditional recommendation, moderate certainty evidence).
- Children with approved DTG dosing (conditional recommendation, low-certainty evidence).
What is the USD 75 a year price?
A pricing agreement was announced on 21 September 2017 at UNGA by the governments of South Africa and Kenya with UNAIDS, the Clinton Health Access Initiative (CHAI), the Bill & Melinda Gates Foundation, Unitaid, DFID, PEPFAR, USAID, and the Global Fund, in collaboration with Mylan Laboratories Limited and Aurobindo Pharma. The agreement, which set ceiling prices for TLD in low- and middle-income countries (LMICs) at an annual cost per person of around US $75 and apply to public sector purchasers and will offer substantial reductions compared with the price of efavirenz-based FDCs.
What is a compulsory license (CL)?
A compulsory license (CL) is an authorization issued by governments allowing the manufacture or import of generic versions of a patented medicine.
CLs are legal provisions in international trade rules and part of most national laws. The rights of World Trade Organization (WTO) member countries to issue CLs is recognized in Article 31 of the WTO’s Agreement on Trade-Related Aspects of Intellectual Property Rights (TRIPS) and has been reaffirmed by the Doha Declaration on TRIPS and Public Health. CLs have been issued in several countries to ensure access to affordable versions of patented medicines. In September 2017, the Malaysian government approved a compulsory license under its Patent Act 1983, on sofosbuvir to procure access to affordable generic treatment for people with hepatitis C.
What about data exclusivity?
Several of the upper middle income countries that are excluded from the Viiv-MPP VL may also have monopolies created by data exclusivity that would prevent the registration of generic DTG in those countries. Where there are no patent barriers in these countries, their governments should waive data exclusivity on DTG to enable registration and import of generic medicines. Where there are patent barriers and data exclusivity, the governments, along with compulsory licenses, should also waive data exclusivity restrictions. In several UMICs, data exclusivity laws or decrees themselves allow waiver in cases of public interest or where a compulsory license is issued.
What provision in the ViiV-MPP VL allows supply under a CL or where there are no patent barriers?
Article 2.4 of the ViiV-MPP licence agreement[13] states: “For avoidance of doubt, it shall not be a breach of the Sublicense for Sublicenses to manufacture, use, sell or supply Products or Raw Materials outside the Territory where such activities would not infringe Non-Territory Patents, including without limitation, where a country outside the Territory has issued a compulsory licence on Non-Territory Patent(s) provided that Sublicensee is authorized to supply such country under the compulsory licence and such use is within the scope of the compulsory licence”.
[1]Algeria, Azerbaijan, Belarus, Brazil, Bulgaria, China, Colombia, Kazakhstan, Mexico, Romania, Russia, and Turkey
[2]https://www.unaids.org/en/resources/documents/2019/gau2019_stateepidemic
[3]https://www.unaids.org/sites/default/files/media_asset/2019-global-AIDS-update_en.pdf
[4]http://www.i-mak.org/wp-content/uploads/2017/06/I-MAKRoadmapSEReportDTG20170619F.pdf
[5]https://medicinespatentpool.org/licence-post/dolutegravir-adult-dtg/
[6]Belarus, Brazil, Bulgaria, China, Kazakhstan, Mexico, Romania, Russia and Turkey.
[7]https://www.unaids.org/en/resources/presscentre/pressreleaseandstatementarchive/2017/september/20170921_TLD
[8]Price for DTG alone, doesn’t include other ARVs to be used with in combination therapy.
[9]https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6248837/
[10]Algeria, Azerbaijan, Belarus, Brazil, Bulgaria, China, Colombia, Kazakhstan, Mexico, Romania, Russia, Turkey.
[11]https://medicinespatentpool.org/licence-post/dolutegravir-adult-dtg/
[12]https://extranet.who.int/prequal/content/prequalified-lists/medicines?label=dolutegravir&field_medicine_applicant=&field_medicine_fpp_site_value=&search_api_aggregation_1=&field_medicine_pq_date%5Bdate%5D=&field_medicine_pq_date_1%5Bdate%5D=&field_therapeutic_area=All&field_medicine_status=&field_basis_of_listing=All
[13]https://medicinespatentpool.org/uploads/2018/08/Second-Amended-and-Restated-Head-Licence-for-DTG-Adults-07.2018.pdf